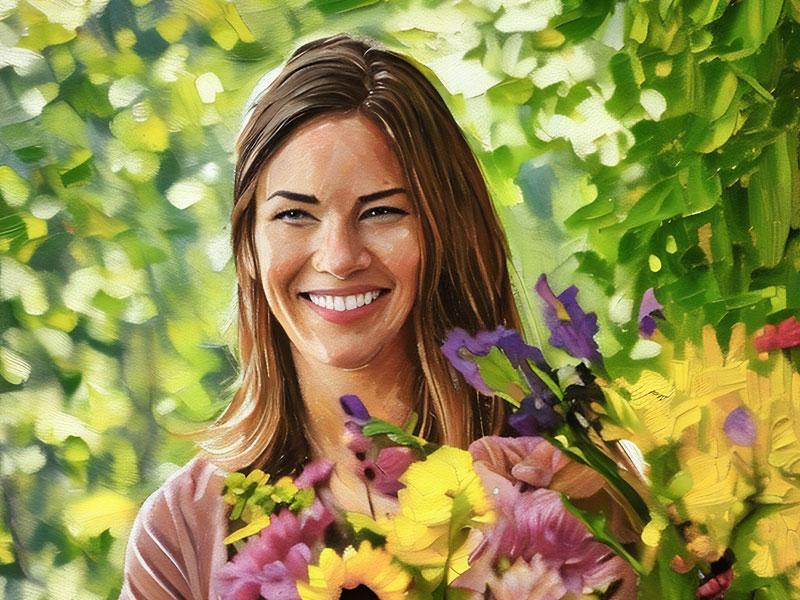
Breakthrough brain tumor treatment gives woman hope for the future
After years of fighting a recurring brain tumor, Amanda Rinehart found herself at another crossroads. First diagnosed at 17, the 32-year-old York native had already endured five surgeries and radiation. When the tumor returned for the third time in 2022, she was determined to explore new options.
On the advice of a co-worker, Amanda sought a second opinion at Penn State Health that would eventually lead her to an innovative, new treatment called GammaTile. The breakthrough therapy targets tumors directly, without the side effects of traditional radiation. She met Brad Zacharia, MD, a Penn State Health neurosurgeon who specializes in brain tumors.
“Right off the bat, he gave me hope,” she said. “He was confident, and his entire team was aware of the latest treatments.”
Amanda and her wife, Jamie Black, were especially impressed with Penn State Health’s team-based approach to care. A multidisciplinary tumor board – made up of experts in neurosurgery, neuro-oncology, radiation oncology, neuroradiology, neuropathology and other specialties – reviewed her case together and reached a consensus on the best path forward.
“When we talked to each doctor, they already knew everything about Amanda, what their plan was and what they would do next,” Jamie said. “It was like a breath of fresh air hearing how many people we had on our side.”
A coordinated plan
Because Amanda was young and otherwise healthy, Dr. Zacharia was confident surgery was a strong first step.
“There are very few types of brain tumors that I deal with where surgery is the end of treatment,” he says. “It’s usually part of the overall plan where patients typically get radiation and, often times, medical therapy.”
After the tumor was successfully removed, Amanda’s doctors recommended chemotherapy with Dawit Aregawi, MD, and radiation with Sean Mahase, MD. Their decision was based on a careful review of her past treatments, recovery progress and the risk of recurrence. They also considered new therapies and clinical trials.
A setback and a new strategy
Despite the aggressive treatment, Amanda’s tumor returned again in September 2024, about eight months after completing chemotherapy.
“We were concerned about the decreasing intervals between surgeries,” Dr. Mahase said. “And this time, the tumor had become more aggressive.”
To minimize risk and preserve healthy brain tissue, her team turned to laser interstitial thermal therapy (LITT), a minimally invasive procedure that uses laser energy to heat and destroy the tumor cells. Amanda began a new round of chemotherapy one month later.
Exploring GammaTile Therapy
While LITT and chemotherapy bought Amanda some time, they weren’t enough to stop the tumor. In March 2025, it returned in the same area once again.
This time, additional radiation posed serious risks because of the damage already done to Amanda’s scalp and surrounding brain tissue. Instead, her doctors proposed a new two-part approach: surgically remove the tumor and implant GammaTiles – small tiles embedded with radioactive seeds designed to safely and precisely target cancer cells from within.
“I wanted to use GammaTile because Amanda’s scalp was fragile due to her prior surgeries and radiation,” said Dr. Mahase. “By placing the GammaTile during surgery, we could start delivering radiation immediately and safely.”
GammaTile delivers about 90% of its radiation within 30 days after it's implanted during tumor removal surgery. The radiation gradually fades until it can’t be detected.
A collaborative effort
Because of the complexity of the procedure, Amanda’s care required collaboration across multiple specialties. Plastic surgeons were brought in to ensure the incision could be safely closed.
“I’ve had so many surgeries, they said it would be hard to close the incision,” Amanda recalled. “But when I look back at pictures, my skin looks like it did after my first surgery –very clean and fresh, like brand new skin.”
Why patients choose Penn State Health
Dr. Zacharia says Amanda’s story reflects why many patients turn to Penn State Health.
“Expert providers, innovative technology, advanced treatments and a high volume of complex cases are all essential to providing optimal care,” he said. “Having all these things has benefited Amanda significantly.”
Looking ahead with hope
Now recovering well, Amanda has started a new inhibitor therapy that blocks signals that help the tumor grow. With minimal side effects from her latest surgery and a strong support team behind her, she feels hopeful.
“I’m really optimistic about the GammaTile and feel like I’m headed in the right direction,” she said. “I’m really grateful that Penn State Health is always pushing for new breakthroughs. I’m not ready for my story to end.”
Brand commercial
There's more to Amanda's story
Advancing patient-centered brain tumor care
Dr. Brad Zacharia's early fascination with the brain made neurosurgery a natural career choice.
Combining clinical skill with deep compassion
Alexa Lantz is a steady source of support and education for patients in their most difficult moments.
Redefining care through compassion and innovation
Dr. Sean Mahase helped build a program that provides a personalized approach to care and leading-edge medicine.








